Chronic diseases like diabetes, hypertension, cancer, and heart disease are significant health concerns—leading causes of illness and death around the world. Effective management of these conditions is crucial for improving patient outcomes and quality of life. One of the most transformative tools in modern healthcare for managing chronic diseases is the Electronic Health Record (EHR). This article explores the role of EHRs in chronic disease management and their impact on long-term patient care.
What are Electronic Health Records (EHRs)?
EHRs are digital versions of patients’ paper charts and include a comprehensive view of patients’ medical histories, diagnoses, medications, treatment plans, immunization dates, allergies, radiology images, and laboratory test results. These records are developed to be shared across healthcare settings, providing a cohesive and integrated patient history.
The Role of EHRs in Chronic Disease Management
- Centralized Information and Accessibility
EHRs offer a convenient and secure way to store and retrieve vital patient information from a centralized platform. This centralization is particularly beneficial for chronic disease management, where continuous monitoring and timely interventions are essential. Healthcare providers can access up-to-date information from any location, ensuring continuity of care even when patients visit different specialists. - Improved Coordination and Communication
Chronic disease management often involves a multidisciplinary approach, requiring coordination between primary care physicians, specialists, nurses, and other healthcare providers. Electronic Health Records (EHRs) facilitate seamless communication and collaboration among healthcare teams, ensuring that everyone unlocks the same knowledge and empowering better choices. - Enhanced Patient Engagement
EHRs often come with patient portals that allow individuals to conveniently access their health information, monitor their progress, take control of their well-being, and communicate with their healthcare providers. This transparency and accessibility empower patients to manage their conditions actively, leading to better adherence to treatment plans and lifestyle changes. - Data-Driven Decision Making
Electronic Health Records (EHRs) contain valuable data that can be analyzed to identify trends, monitor disease progression, and evaluate the effectiveness of treatments. Healthcare providers can use this data to make evidence-based decisions, customize treatment plans for individual patients, and adjust interventions as necessary. - Proactive Management and Early Intervention
One critical benefit of EHRs is the ability to set up alerts and reminders for routine screenings, vaccinations, and follow-up appointments. These proactive measures ensure that patients care for themselves and lower the likelihood of associated complications. - Telemedicine Integration
The integration of telemedicine with EHRs has further revolutionized chronic disease management. Patients can have virtual consultations with their healthcare providers, share real-time health data from wearable devices, and receive medical advice without needing in-person visits. This convenience is primarily for individuals with mobility challenges or those residing in secluded regions.”
Case Studies and Success Stories
- Diabetes Management
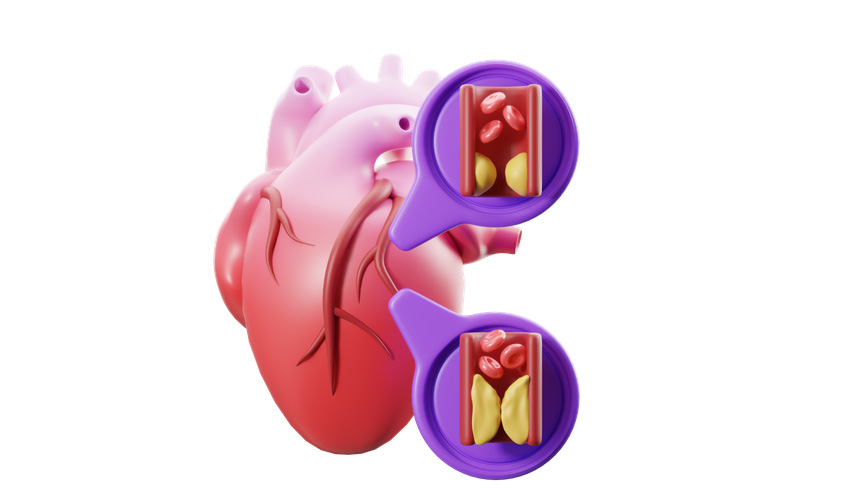
In diabetes care, EHRs have proven invaluable in tracking blood sugar levels, monitoring medication adherence, and managing comorbid conditions. For instance, EHRs in an extensive healthcare system improved glycemic control and reduced hospitalizations for diabetic patients. The ability to analyze trends in blood sugar levels and adjust treatment plans accordingly has led to better overall management of the disease. - Hypertension Control
EHRs have also shown significant benefits in managing hypertension. Through regular monitoring and automated reminders for blood pressure checks, patients are more likely to maintain their target blood pressure levels. Studies have demonstrated that using EHRs in hypertension management programs leads to better blood pressure control and a lower risk of cardiovascular events.
Challenges and Considerations
While EHRs offer many benefits for managing chronic diseases, they also have some challenges. These include issues with data privacy, interoperability between different EHR systems, and the learning curve associated with new technology. Healthcare providers must tackle these challenges head-on to deliver the best possible care.
Conclusion
Electronic Health Records (EHRs) have revolutionized chronic disease management. They provide centralized, accessible, and comprehensive patient information, improving coordination and communication among healthcare providers. EHRs empower patients, enable data-driven decision-making, and support proactive care. Integrating EHRs with other digital health tools as technology evolves will further enhance chronic disease management and long-term patient care. These innovations can enable healthcare systems to pursue improved outcomes and elevate patient quality of life.
By understanding and leveraging the capabilities of EHRs, healthcare providers can continue to make significant strides in chronic disease management, ultimately leading to healthier and more empowered patient populations.